Treatment & Monitoring
TURBT
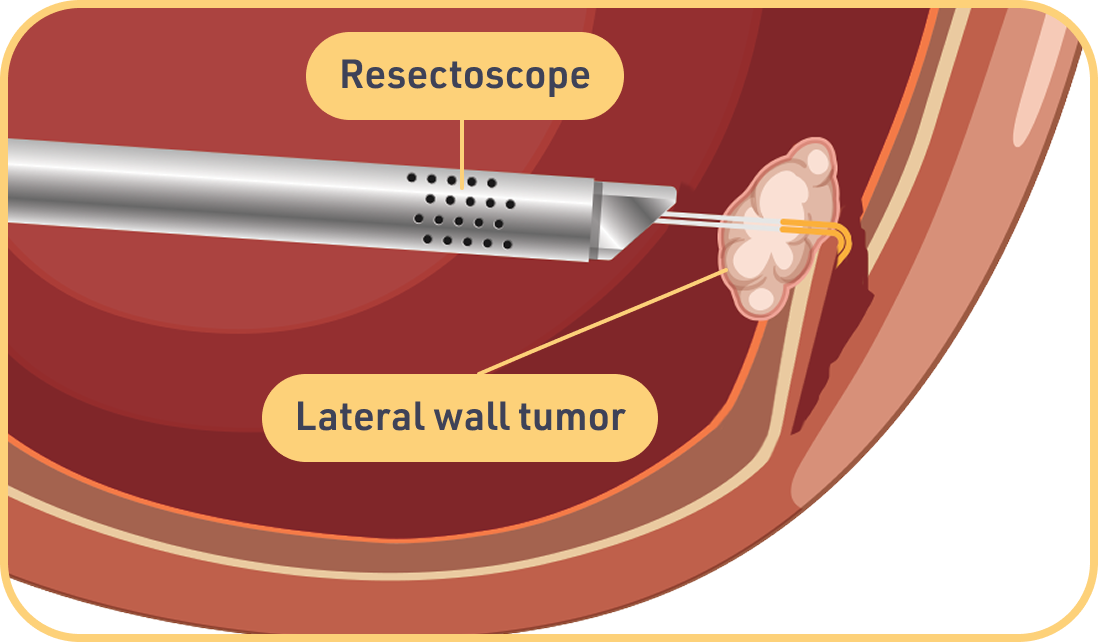
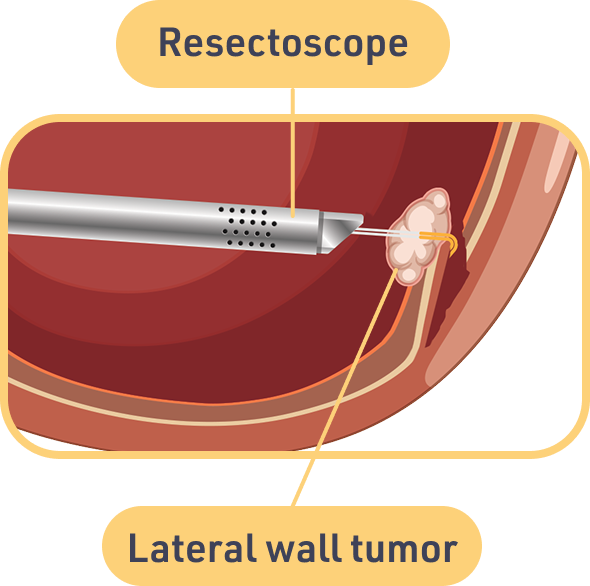
The term TURBT stands for transurethral resection of bladder tumor. TURBT is a surgical procedure used to remove tumors from the bladder. This is done to collect cells to be analyzed in diagnosing bladder cancer, called a biopsy. It is also the most commonly used treatment to remove all visible tumors from the lining of the bladder. The procedure generally takes about an hour and is usually performed in the hospital as an outpatient procedure.
Preparing for TURBT
Before you undergo TURBT, your doctor will give you directions to follow to prepare for the procedure. You will likely be told not to eat or drink anything for 8 hours before TURBT. Your doctor will definitely want to know if you take blood thinners, including aspirin, NSAIDs, or anticoagulants. This is because these drugs can increase the risk of bleeding during surgery. It's recommended that you bathe before the TURBT procedure. Finally, you will want to arrange for someone to drive you home after the procedure.
During TURBT
You will receive anesthesia before the TURBT procedure so that you will not feel any pain. You may receive general anesthesia, where you will be asleep, or regional anesthesia where you will be awake during the procedure, but the lower part of your body will be numb.
For the actual surgery, your doctor will insert the scope through your urethra (the tube that carries urine out of the body from your bladder) and into your bladder. At the end of the scope is a small wire loop that uses electrical current to remove tumors and cauterize the resulting wounds to prevent bleeding. After the surgery, the scope and the tumors will be removed. The doctor might then insert a catheter into your bladder. It's used to drain urine (pee) and other fluids from the bladder and help prevent blood clots, but not everyone needs a catheter. The entire procedure generally will last about 1 to 1.5 hours, depending on what your doctor finds and how much tumor needs to be removed.
Recovering from TURBT
Most people can go home the same day they have TURBT, although it may take a few days to a few weeks to recover completely from the surgery. While recovering, you should follow any instructions your doctor has given you. It's good to keep your bladder from getting full. It's also helpful to stay well hydrated to help flush the bladder.
Here are some symptoms that are common after TURBT:
- Painful urination
- Bladder irritation
- Frequent urination
- Bladder spasms
- Blood in urine
Sometimes more serious side effects occur. These can include an inability to urinate, fever and/or chills, nausea and vomiting, or heavy bleeding or blood clots. If you experience any of these, you should reach out to your doctor.
Some tumors are hard to remove completely with TURBT. Some may not even be visible. Also, TURBT can create floating tumor cells that might attach to the bladder lining, causing the cancer to return. For these reasons, your doctor may recommend adding intravesical treatment (IVT) after TURBT. This procedure involves placing medicine inside the bladder to help kill cancer cells that might still be there. In the case of intermediate-risk or high-risk bladder cancer, the treatment guidelines* generally recommend adding IVT.
*Guidelines consulted include America Urological Association/Society of Urologic Oncology and National Comprehensive Cancer Network.
IVT (intravesical therapy)
IVT means the medicine is given through a urinary catheter inserted into the bladder. After the medication is in the bladder, patients must hold it there for 1 to 2 hours. Sometimes patients are asked to shift their position every 15 minutes. This is to help the drug coat the entire inside of the bladder. IVT is generally used as adjuvant therapy, which means it is added after the main treatment to enhance the effects.
There are 2 categories of medicines that are used most often in IVT: immunotherapy and chemotherapy.
IVT Immunotherapy (BCG)
Immunotherapy is a treatment that boosts the ability of your immune system to fight cancer. The immunotherapy used as adjuvant therapy in NMIBC is BCG (Bacillus Calmette-Guerin), which triggers the immune system to attack bladder cancer cells. This is used after TURBT to help prevent the cancer from coming back.
The BCG treatment schedule is 1 intravesical instillation per week for 6 weeks (this is called induction). BCG is typically given in your doctor's office. Some patients need more than 1 course. Your doctor will discuss the full treatment schedule with you. BCG is an effective treatment for bladder cancer, but BCG is not recommended for patients who are immunocompromised (have a weakened immune system).
Common side effects can include:
- Flu-like symptoms
- Burning feeling in the bladder
- Need to urinate often
- Blood in the urine
If you are tumor free after treatment, your doctor may suggest you continue receiving the drug on a maintenance schedule for 1 to 3 years. This schedule is less frequent than an induction schedule.
IVT Chemotherapy
There are 2 ways intravesical chemotherapy is used: One way is when a single intravesical dose is given immediately after TURBT. This is called perioperative use. The other way is as adjuvant therapy. Similar to IVT immunotherapy, it will be given as 1 intravesical instillation per week for 6 weeks. Your doctor will discuss the full treatment schedule with you.
Mitomycin C and gemcitabine are the most common chemotherapy drugs used for IVT. They are usually given after the initial TURBT to help stop cancer cells from coming back and lower the recurrence rate. Since chemotherapy is given inside the bladder only, it does not impact your entire body. As a result, you will not have many of the side effects that chemotherapy often causes, such as hair loss.
Common side effects can include:
- Skin irritation
- Burning feeling in the bladder
- Blood in the urine
If you are tumor free after treatment, your doctor may suggest you continue receiving the drug on a maintenance schedule for 1 year. This schedule is less frequent than an induction schedule.
After Treatment
After you complete your treatment, you will be monitored for a period of time.
- For intermediate-risk bladder cancer, American Urological Association guidelines recommend you see your doctor every 3 to 6 months for 2 years at the start.
- During the third and fourth years, this follow-up will decrease to every 6 to 12 months, and after that, once a year.
Studies have shown that IVT after TURBT helps to keep cancer from coming back. However, the nature of NMIBC, especially LG-IR-NMIBC, is that it will come back in many cases. If your cancer does return, you will probably undergo TURBT again. Sometimes a patient may need to undergo TURBT several times.
NMIBC treatments have not changed much in more than 30 years, but new approaches are now being studied. If your cancer comes back, research your options and talk with your doctor about what new treatments might be available for you.

ADVANCEMENTS IN BLADDER CANCER TREATMENT
In recent years, science has made progress in developing new treatments for bladder cancer. In fact, clinical trials are now underway to explore new options for treating LG-IR-NMIBC.
Complete the form below to receive up-to-date information on NMIBC, new resources and UroGen treatments.